Our Health Library information does not replace the advice of a doctor. Please be advised that this information is made available to assist our patients to learn more about their health. Our providers may not see and/or treat all topics found herein.
Topic Contents
Blocked Tear Ducts
Condition Basics
What is a blocked tear duct?
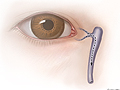
Tears normally drain from the eye through small tubes called tear ducts, which stretch from the eye into the nose. If a tear duct becomes blocked or fails to open, tears cannot drain from the eye properly. The duct may fill with fluid and become swollen, inflamed, and sometimes infected.
Blocked tear ducts happen most often in babies, though they may occur at any age.
Most of the time, blocked tear ducts in babies clear up on their own by the time your child is 6 months old. They usually have no effect on the baby's vision or cause any lasting eye problems.
What causes it?
Causes of blocked tear ducts in children include:
- Failure of the thin tissue at the end of the tear duct to open normally. This is the most common cause.
- Infections.
- Abnormal growth of the nasal bone that puts pressure on a tear duct and closes it off.
- Closed or undeveloped openings in the corners of the eyes where tears drain into the tear ducts.
In adults, blocked tear ducts may be caused by an injury to the bones or tissues around the eyes or by another disorder, sometimes related to aging. For example, a blocked tear duct may result from a thickening of the tear duct lining, abnormal tissue or structures in the nose, or problems from surgery on or around the nose.
What are the symptoms?
Symptoms often affect only one eye. They may include:
- Heavy tearing. This may range from the eye looking wet to having tears run down the cheek.
- A yellow or white buildup in the corner of the eye. The eyelids may stick together.
- Redness and swelling around the eye or nose. This can be caused by infection in the eye's drainage system, such as dacryocystitis. In severe cases, infection can spread to the eyelids. A severe infection can cause fever, pain, increased redness and swelling, and mucus or pus in the eye.
Babies who have blocked tear ducts usually have symptoms within the first few days to the first few weeks after birth.
The symptoms of a blocked tear duct may get worse after an upper respiratory infection, such as a cold or sinus infection. Wind, cold, and sunlight also may make symptoms worse.
How is it diagnosed?
A blocked tear duct is diagnosed based on a medical history and physical exam. The doctor may also use tests to measure the amount of tears or to see if tears are draining normally from the eyes. Other tests can help your doctor find out where the blockage is or how it was caused.
How is a blocked tear duct treated?
Most babies who have blocked tear ducts don't need treatment. A doctor can suggest ways to help prevent infection and other problems until the blockage goes away. If signs of infection develop, your baby may need antibiotics.
Sometimes a probing procedure may be done to open the duct if the duct doesn't clear on its own. Talk to your doctor to see if probing will help. In rare cases, babies with blocked tear ducts have a more severe problem that requires more complex surgery.
In adults who have blocked tear ducts, treatment depends on the cause of the blockage. If the duct is blocked because of a long-term infection, antibiotics may be used. Surgery may be needed for structural problems or abnormal growths. Probing usually isn't done for adults.
How can you care for your child at home?
- Keep your child's eye clean.
- Moisten a clean cotton ball or washcloth with warm (not hot) water, and gently wipe from the inner (near the nose) to the outer part of the eye. With each wipe, use a new or clean part of the cotton ball or washcloth.
- If your child's eyelashes are crusty with mucus, clean them with a moist cotton ball using a gentle, downward motion. If the eyelids get stuck together, place a clean, warm, wet cotton ball over that eye for a few minutes to help loosen the crust.
- Always wash your hands before and after you touch the eye area.
- If your child's doctor suggests it, gently massage the area of the blockage. This can help prevent fluid buildup in the duct. Make sure that your hands are clean and your nails are short.
- If the doctor prescribed antibiotic pills, eyedrops, or ointment for your child, give them exactly as directed. Do not stop using them just because your child's eye gets better. Your child needs to take the full course of antibiotics.
- To put in eyedrops or ointment:
- Tilt your child's head back, and pull the lower eyelid down with one finger.
- Drop or squirt the medicine inside the lower lid.
- Do not touch the ointment or dropper tip to the eyelashes or any other surface.
- If the tearing bothers your child, try to limit their time in the wind, cold, and sunlight.
Related Information
Credits
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use and Privacy Policy. Learn how we develop our content.
To learn more about Ignite Healthwise, LLC, visit webmdignite.com.
© 2024 Ignite Healthwise, LLC. Healthwise, Healthwise for every health decision, and the Healthwise logo are trademarks of Ignite Healthwise, LLC.